European intensive care nurses shadow Swedish colleagues: ‘We are bringing home a wealth of ideas

Recently, Karolinska University Hospital hosted five intensive care nurses from Belgium, Italy, Germany, Austria, and the Netherlands. For two weeks, the visiting nurses shadowed their Swedish colleagues in the intensive care units and took part in training and simulations.
“It has been inspiring to design this project from the very beginning and to see how well it has worked in practice. The participants arrived without any prior knowledge of our routines, yet quickly adapted and contributed in meaningful ways,” says Camilla Smedberg, Emergency Preparedness Coordinator at Karolinska University Hospital who prepared the two-week program togehter with her colleauges Johanna Rydström, Care Team Manager for the Peri-Operative Medicine & Intensive Care Function (PMI).
Smedberg is also responsible for several of the programme’s e-learning modules and simulation exercises. Her colleague Pauline Rylander Hagson, Head of Unit at PMI, is part of EUHA’s Nursing network togehter with Katarina Meijers. She notes that the exchange has revealed many common challenges:

“A changing world requires us to be better prepared – not only for pandemics but also for workforce challenges and the need to support each other across borders in times of crisis. This kind of collaboration simply did not exist before. With this project we want to break down barriers.”
Both Smedberg and Rylander Hagson stress that the exchange is bilateral, offering valuable insights for everyone involved. “Every healthcare system is different, but listening to diverse perspectives is invaluable. We see how teamwork, roles, and hierarchies vary across countries, and those insights are just as important as the clinical training,” says Smedberg.
The fellowship has already created strong networks that extend beyond the programme. Next, Swedish nurses will travel to partner hospitals across Europe to continue the exchange. Petter Ekvall and Mikaela Hansdotter, intensive care nurses at Karolinska, are among those preparing for their visits.

“This has been a great opportunity to hear what our colleagues think about our organisation, especially our staffing model and the role of assistant nurses. Now we look forward to seeing how intensive care is organised in their hospitals and how they approach disaster preparedness,” says Ekvall.
Hansdotter adds: “This is a unique chance to learn how intensive care is delivered in different countries, to share knowledge, and to gain a deeper understanding of both differences and similarities. Meeting motivated and positive colleagues who work towards the same goals has been truly inspiring.”
Five voices from European colleagues
Martin Eicher, Charité Universitätsmedizin, Berlin

“I want to contribute to the exchange between European intensive care nurses and learn more about disaster preparedness in intensive care, as well as the respective plans at university hospitals across Europe. At Karolinska, I found a high level of pandemic preparedness and impressive nursing competence. The best part of my profession? Having direct contact with patients and working in an environment where teamwork is essential. Intensive care is constantly developing, and continuous learning is necessary.”
Sara Di Leo, San Raffaele Hospital, Milan

“I enjoy being part of a team, even when we come from different regions of Europe. This collaboration helps us keep an open mind and manage emergencies across borders. I am taking home many new ideas from Karolinska, especially around teamwork – there is time set aside for discussion and sharing views between nurses, physicians, and assistant nurses. I saw collaboration and communication in every situation. The best part of my profession? Making a real difference thanks to our knowledge, experience, and constant drive to improve and look ahead.”
Frans Vanwingh, UZ Leuven, Leuven

“In Belgium we have faced several disasters in recent decades, including the 2016 terrorist attacks, industrial explosions, and large-scale fires. At Karolinska, I was able to observe the work in detail, ask questions, and exchange experiences. I will bring home ideas such as multidisciplinary SBAR handovers, structured briefings with time to listen, the importance of breaks even during minor procedures, and the strong involvement of assistant nurses. The best part of my profession? Being part of a team that treats the most critically ill patients and gives them a second chance at life.”
Paul Fassl, Allgemeines Krankenhaus, Vienna

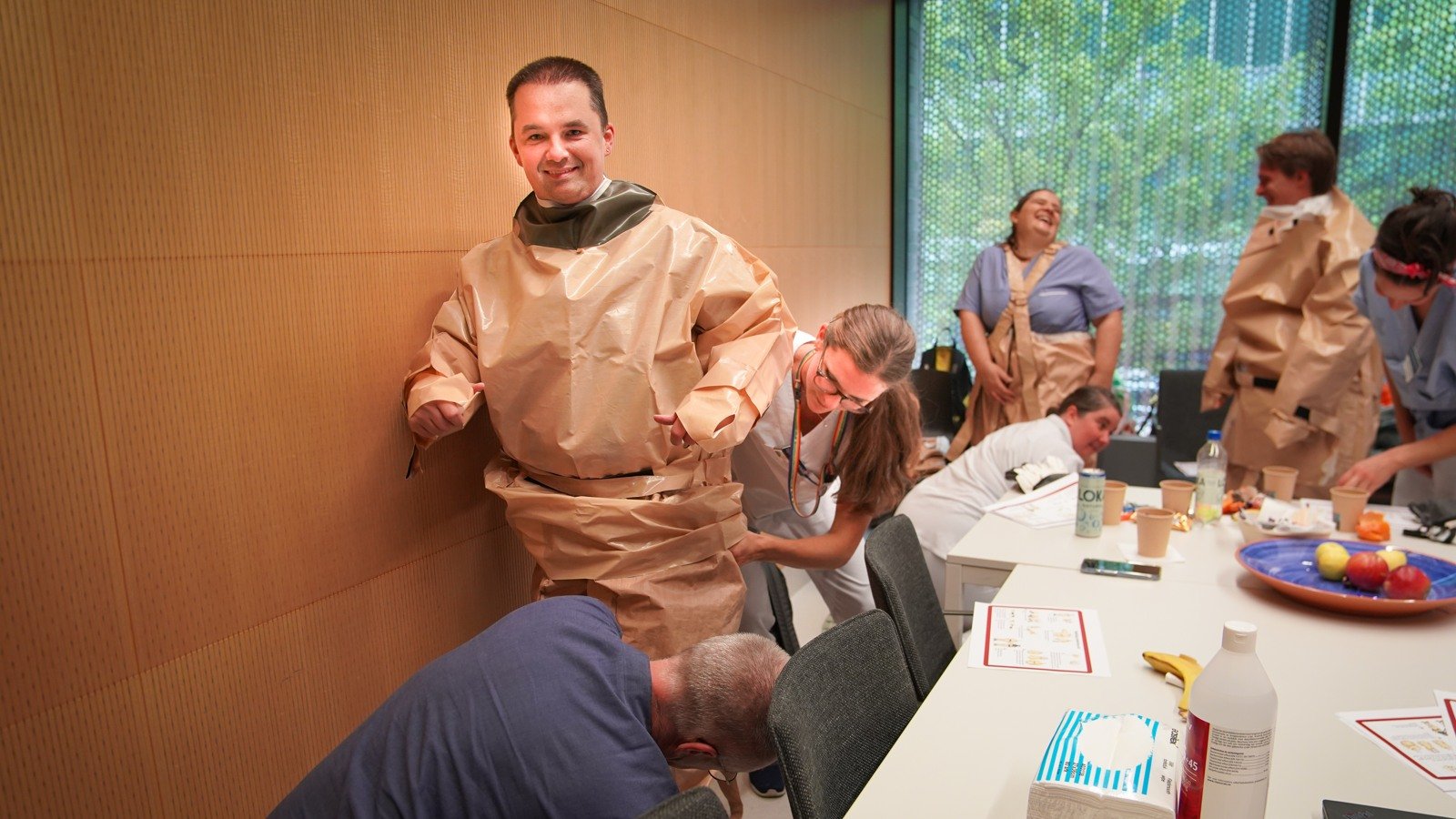
Paul Fassl (center) practicing putting on protective gear ahead of a simulation exercise.
“I applied to the EUCARE programme to learn about nursing practices in other EU countries. My time at Karolinska highlighted the importance of evidence-based nursing, specialised education, and training. I was impressed by the number of specialised nurses working every day to improve quality of care. The simulation exercises were particularly valuable, and I gained new insights into disaster preparedness. The best part of my profession? Working in the dynamic environment of intensive care, where one must stay up to date with medical and nursing advances. It makes the work both varied and stimulating.”
Michaël Daniels, Erasmus MC, Rotterdam
“I see EUCARE as a chance to learn from experts in different European healthcare systems, exchange knowledge, and bring back new insights and evidence-based practices to my own workplace. Beyond clinical expertise, I also want to develop my leadership, communication, and teamwork skills. From Karolinska, I will take home the importance of clear role distribution, standardised communication, and strict adherence to safety protocols as the foundation of high-quality intensive care. The best part of my profession is the human side – supporting patients and their families through some of their most difficult moments. It is truly meaningful.”
Text and photo: Nneka Magnusson Amu